By Dorothy H. Crawford
It is over 100 years since HIV, the AIDS virus, began spreading in humans. It all started in West Central Africa where, scientists calculate, HIV jumped from chimpanzees to humans around 1900. Then in 1964 the virus made its first trans-continental flight. In one move it leaped from Kinshasa, capital of the Democratic Republic of Congo, to the Caribbean island of Hispaniola. Here it established a foot-hold in Haiti before travelling on to the US in 1969. So began a journey that took HIV to virtually every country in the world, eventually infecting 65 million people, a figure that is rising by around three million annually.
Without a doubt the best way to halt this spread is with a vaccine against HIV but none of the many preparations tested so far is effective. The bad news is that we are still decades away from having a licensed vaccine, so is there any good news to impart?
Startling headlines earlier this year reported a breakthrough – a so-called ‘functional cure’ in an HIV positive baby. Surprisingly, the report came from the US where all pregnant women should get antenatal HIV screening. Nevertheless, this particular mother slipped through the net. She was unaware of her HIV infection until she tested positive during labour – too late to give her antiviral drugs to prevent virus transmission to the baby. So doctors gave the baby a course of antivirals, starting within 30 hours of birth. Although he/she initially tested positive for HIV, this soon became undetectable. After 18 months the treatment was discontinued, a process that usually causes the virus to bounce back. But in this case only traces of HIV were detectable after the treatment stopped. So although the drugs had not eliminated the virus completely, doctors think that the child’s immune system can now control the infection so that even without antivirals he/she will remain healthy and will not infect others.

This case may be a one off but around the same time French researchers reported similar ‘functional cures’, this time in adults. Fourteen of 70 patients given antivirals within 2 months of their initial HIV infection maintained undetectable virus loads that did not bounce back after stopping the drugs.
No one knows exactly how these functional cures occur or why they are restricted to a minority of those treated. Yet these two reports highlight the fact that early treatment benefits individuals infected with HIV and can also be used to block another loophole in our armament against the virus – that is, early transmission.
Early after infection, when people feel well and are unaware that HIV is silently invading their bodies, the viral load in the blood and body fluids is extremely high. The combination of unawareness and high levels of circulating virus means that this is the time when the virus is most likely to be spread to others. So early diagnosis followed by antiviral treatment is the key to plugging this virus transmission route. This requires frequent testing of people at high risk of infection and one solution is to allow wider access to HIV testing kits, for example in gay clubs, saunas, and at home – situations that are all presently on trial in the UK and elsewhere.
Other suggestions for curtailing HIV spread to people at very high risk, such as those with HIV positive sexual partners, are pre- or post-exposure prophylactic antivirals. The former mirrors the routine use of anti-malaria drugs for healthy travellers to malaria infested areas while the latter is modelled on the morning after contraceptive pill.
Obviously, without a vaccine, winning the fight against this rogue virus requires a multipronged approach using as many prongs as possible. We must not be complacent. We should acknowledge and build on the landmark introduction of highly active antiviral therapy in the 1990s that transformed the outlook of people living with HIV. Before this date HIV infection was a sure death sentence, afterwards virus carriers could expect a normal life span. Now we are learning how to use these drugs to achieve functional cures and effective preventative measures. Clearly much more needs to be done but the battle against HIV is well under way.
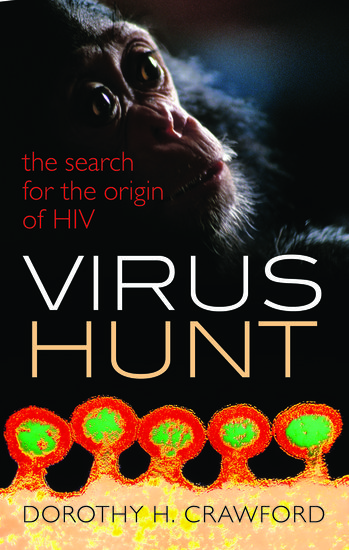
Dorothy H. Crawford has been Assistant Principal for Public Understanding of Medicine at the University of Edinburgh since 2007. Her books include The Invisible Enemy (OUP, 2000), Deadly Companions (OUP, 2007), Viruses: A Very Short Introduction (OUP, 2011), and Virus Hunt (OUP, 2013). She was elected a Fellow of both the Royal Society of Edinburgh and the Academy of Medical Sciences in 2001, and awarded an OBE for services to medicine and higher education in 2005. She has written several previous articles for the OUPblog.
Subscribe to the OUPblog via email or RSS.
Subscribe to only health and medicine articles on the OUPblog via email or RSS.
Image credit: AIDS ribbon by Amada44. Image available via WikiCommons.

Recent Comments
There are currently no comments.